Signs & Symptoms
The classic symptoms of bubonic plague appear suddenly, often within 2 to 6 days after exposure. Early signs include:
- Fever: High fever is one of the first signs of infection, often reaching 39–41°C (102–105°F).
- Chills: Accompanying the fever, patients often experience intense chills.
- Headache and muscle aches: These can be severe, similar to flu-like symptoms.
- Lymphadenopathy (Buboes): Painful, swollen lymph nodes (called “buboes”) are a hallmark sign of bubonic plague. These typically occur in the groin, armpit, or neck and are often tender to the touch. The buboes can become very large and may rupture in severe cases.
If the infection progresses, it can lead to more severe forms of plague:
- Septicemic plague: This occurs when the bacteria spread to the bloodstream, leading to symptoms such as bleeding under the skin, abdominal pain, vomiting, and diarrhea. Gangrene can also develop, particularly in the extremities (fingers, toes, or nose), which may turn black and necrotic.
- Pneumonic plague: This is a particularly deadly form of plague that affects the lungs and can be transmitted from person to person through respiratory droplets. Symptoms include cough, chest pain, difficulty breathing, and sometimes blood-tinged sputum. Pneumonic plague is often fatal within 24–72 hours if left untreated.
Diagnosis
Historically, diagnosis of bubonic plague was primarily clinical, based on the observation of symptoms, particularly the presence of buboes. The rapid onset of fever, chills, and swollen lymph nodes, along with the patient’s recent history of exposure to infected animals or fleas, provided key clues. However, in modern medicine, diagnostic techniques have advanced significantly:
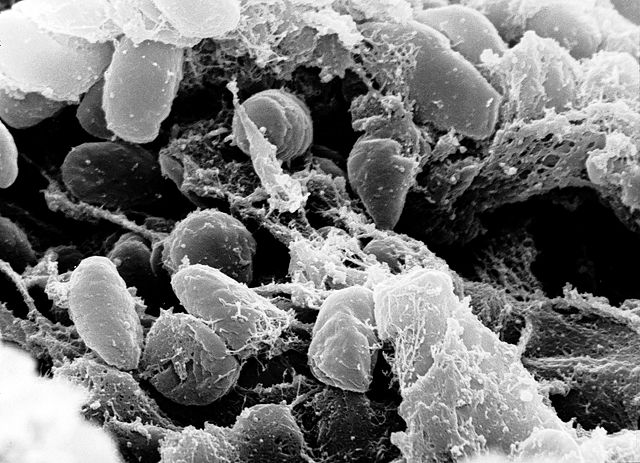
- Laboratory diagnosis: Confirmation of the diagnosis requires microbiological testing. Blood cultures, tissue biopsies, and sputum cultures can be used to identify the bacterium Yersinia pestis.
- Polymerase chain reaction (PCR): PCR testing is a highly sensitive and specific method to detect the genetic material of Y. pestis, even in the early stages of infection.
- Serological tests: These tests detect antibodies against Y. pestis in the blood, indicating past exposure or infection.
Early diagnosis is crucial, as plague can progress rapidly, and without prompt treatment, it can be fatal. In the case of suspected pneumonic plague, tests to identify respiratory pathogens may be done to rule out other conditions.
Treatment
Historically, treatment for bubonic plague was limited and largely ineffective. The medieval approaches were based on superstition and rudimentary medicine, including:
- Bloodletting: A common practice at the time, bloodletting was used to "balance" bodily fluids, although it had no real effect on the infection.
- Herbal remedies: Various plants and herbs were used in attempts to treat the plague, such as garlic, vinegar, and a variety of poultices.
- Quarantine: The most effective historical measure was quarantine, where infected individuals and their contacts were isolated to prevent further spread. This was rudimentary but, in some cases, helped limit the spread of infection.
In modern times, antibiotics are the cornerstone of treatment:
- Antibiotics: Drugs such as streptomycin, doxycycline, and ciprofloxacin are highly effective in treating bubonic plague when administered early. The mortality rate can be as low as 1% with proper treatment, compared to 60–90% in untreated cases.
- Supportive care: In severe cases, supportive care such as intravenous fluids, oxygen, and pain management is provided to help patients recover.
- Vaccination: A vaccine for the plague was developed in the late 19th century and has been used in some high-risk areas for prevention. However, due to the relatively low incidence of plague today, routine vaccination is not common. Ongoing research aims to improve vaccine efficacy, especially in areas where plague remains a threat.